Abstract
Background Primary mediastinal B-cell lymphoma (PMBCL) is a distinct clinicopathologic entity with a predilection for female adolescents and young adults (AYAs). Due to its rarity, there is a paucity of prospective data and lack of randomized studies to inform on optimal frontline therapy. Expert guidelines from around the globe vary considerably with recommendations ranging from dose-intensive chemoimmunotherapy (CIT) to R-CHOP-21 with consolidative mediastinal radiation (RT). To assess if there are distinct differences in outcome between these approaches, we performed a systematic review and meta-analysis comparing dose-intensive versus standard CIT for the frontline treatment of PMBCL.
Methods We performed a comprehensive and specific literature search on the frontline treatment of PMBCL. Studies included in our meta-analysis were prospective or retrospective published datasets that reported treatment outcomes (event free survival, EFS; progression free survival, PFS; overall survival, OS) for specific CIT regimens for PMBCL patients of any age. Standard approach was defined as R-CHOP-21 or CHOP-21, with or without RT. Dose intensive approaches were defined as regimens that increase the frequency, dose or number of systemic agents in comparison to R-CHOP-21. Case reports, small case series (<5 PMBCL patients) and unpublished conference abstracts were excluded. We searched MEDLINE, Embase, and Cochrane CENTRAL via Ovid and Web of science for all published literature on this topic on February 8th, 2022. This study followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guideline and the PRISMA extension statement.1 Two independent authors screened all studies to compile a final list of included publications, from which data was extracted. Patient number, trial type, treatment, consolidative RT/autologous stem cell transplant (auto-SCT), EFS, PFS and OS data was collected from each study. Pooled analysis for each efficacy outcome was calculated using percentages and sample size. Linear regression was used to compare treatment modalities for EFS, PFS and OS outcomes. Median follow-up time varied for each study, therefore outcomes were standardized by calculating average yearly event-free percentages.
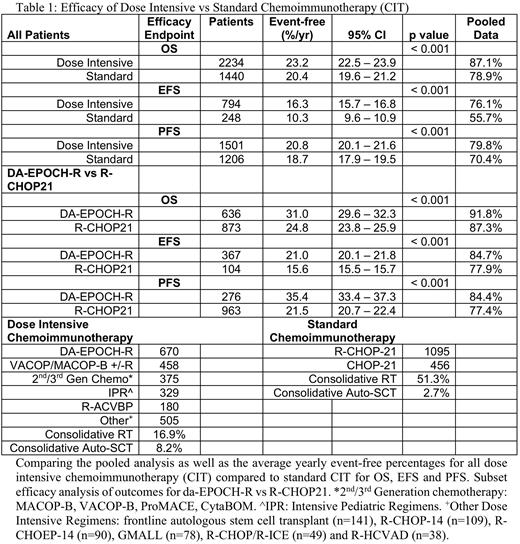
Results Our systematic review generated 1404 articles, which led to the inclusion of 53 publications, encompassing 4068 patients. 2517 patients were treated with dose-intensive approaches compared to 1551 with standard R-CHOP-21 (n=1095) or CHOP-21. Dose intensive approaches are summarized in Table 1. Consolidative RT was administered in 16.9% of the dose intensive arms, compared to 51.3% of R-CHOP regimens. Median follow up across all studies was 56 months.
Outcome data is summarized in Table 1. 2234 patients in the dose intensive studies were evaluable for OS, with a cumulative 87.1% reported survival. Standard CIT studies reported 1440 patients with OS data, with a combined 78.9% reported survival. Controlling for differences in median follow up, the average percent per year surviving in the dose intensive CIT arm was 23.2% (95% CI 22.5 - 23.9) compared to 20.4% (95% CI 19.6 - 21.2) for standard CIT (p < 0.001). Aggregate overall survival and percent per year surviving for DA-EPOCH-R patients alone was 91.8% and 31.0% (29.6 - 32.3), compared to 87.3% and 24.8% (23.8 - 25.9; p < 0.001) for R-CHOP-21. Collective data revealed an EFS of 76.1% (n=794) and a PFS of 79.8% (n=1501) for the dose intensive group, compared to 55.7% (n=248) and 70.4% (n=1206) for the standard CIT arm. Improved EFS and PFS in the dose-intensive arm was confirmed with average percent per year event free survival (EFS 16.3% vs. 10.3%, p < 0.001; PFS 20.8% vs 18.7%, p < 0.001) for all patients, as well as the subgroup of DA-EPOCH-R compared to R-CHOP-21 (EFS 21.0% vs 15.6%, p < 0.001; PFS 35.4% vs 18.0%, p < 0.001).
Conclusion To our knowledge, this is the largest meta-analysis reported to date of efficacy outcomes for frontline CIT in PMBCL. Pooled and yearly event-free analyses demonstrate that dose intensive approaches have more favorable overall survival, EFS and PFS. Furthermore, fewer patients in the dose intensive arm are exposed to consolidative RT, curtailing chronic toxicity. As we await results of randomized prospective trials, our meta-analysis supports the use of dose-intensive chemoimmunotherapy alone for the initial management of PMBCL.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal